Founded by healthcare attorneys with 70 + years of Combined Experience
Developed by Health Care Professionals for Health Care Professionals
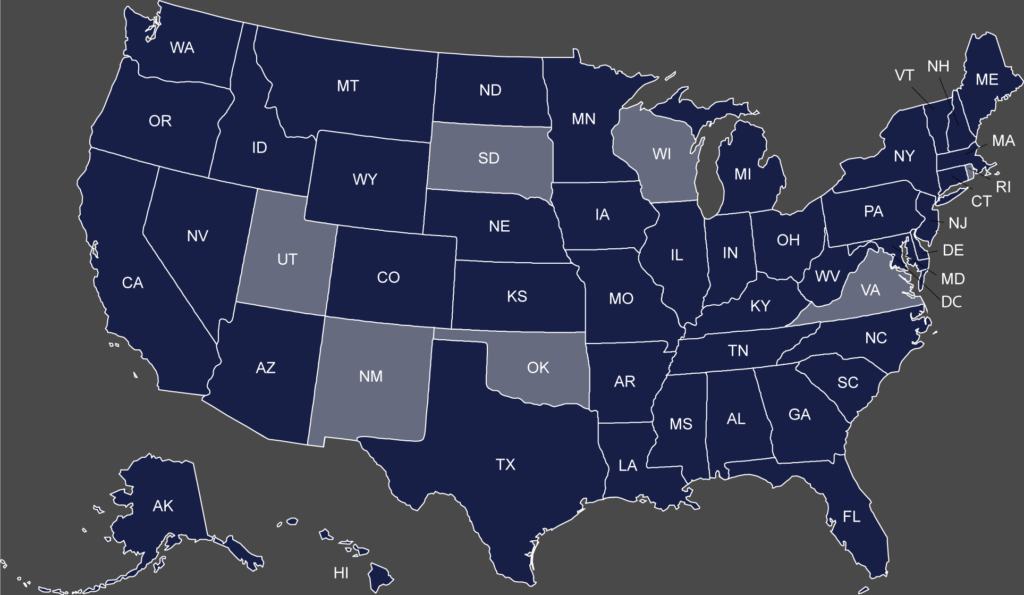
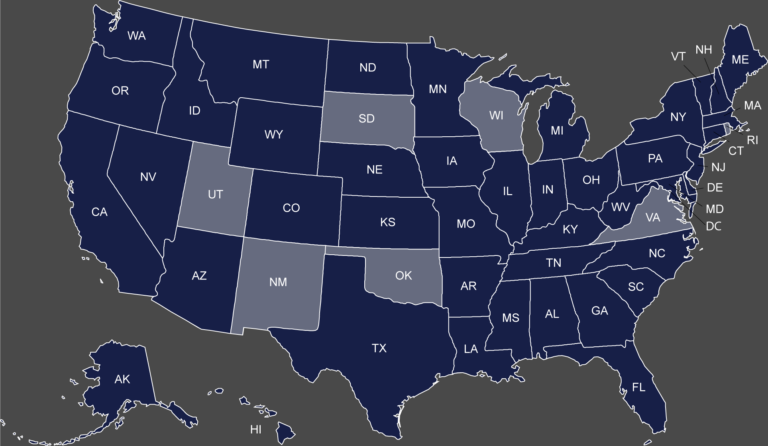
A provider-focused approach to exclusion screening. Supporting your Federal and State screening obligations in a simple, reliable and cost-effective way.
Comprehensive Exclusion Screening Solutions.
Our Services
Our services provide end-to-end exclusion screening to help you stay compliant with federal and state regulations. We offer tailored solutions to safeguard your organization, ensuring you avoid penalties and protect your reputation.
An extensive clientele.
our Customers
- Hospitals
- Medical Centers
- Physician Practices
- Dental Practices
- Laboratories
- PT/ OT/ ST Provider
- Behavioral Health Providers
- Health Care Supply Companies
- Medicaid Advantage Plans
- State and Country Health Departments
- DME Suppliers
- Health Care Consultants
- Law firms
- Billing and Staffing Companies
Our Founders
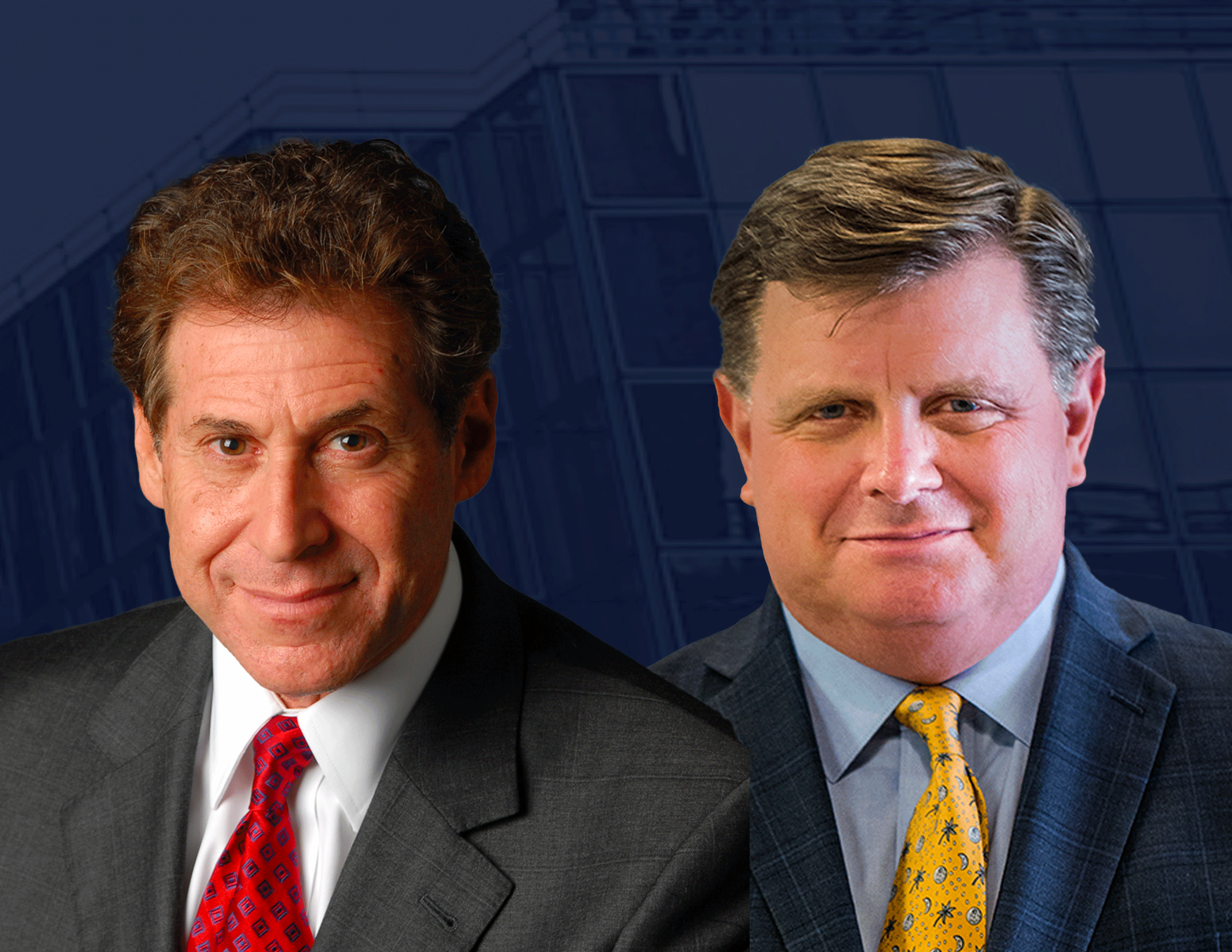
Paul Weidenfeld & Robert W. Liles
Exclusion Screening, LLC was established by healthcare attorneys Robert Liles and Paul Weidenfeld, both of whom are former DOJ National Health Care Fraud Coordinators. Drawing on their deep understanding of the challenges faced by providers and the critical importance of regulatory compliance, Robert and Paul set out to create a simple, cost-effective solution for fulfilling Federal and State exclusion screening requirements. Exclusion Screening, LLC achieves this by conducting monthly checks to verify the exclusion status of all employees, vendors, and contractors across all Federal and State exclusion lists.
Paul Weidenfeld
Robert W. Liles
FAQ
Frequently Asked Questions
Exclusion Screening FAQs
What is an OIG Exclusion?
How Often Should Screening be done?
Who Should be Screened? Who are Providers Required to Screen?
Company FAQs
How often is Exclusion Screening’s exclusion database updated?
Which exclusion lists are included in Exclusion Screening’s package?
May I have multiple users?
Articles and Resources
Featured Articles
Stay Connected
Recent Posts
Ensure Compliance -
Talk to Us
Schedule a Demo of our Exclusion Screening or Compliance Hotline Services!